This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 70 year old male who is a daily wage labourer by occupation was brought to the casualty ward with the chief complaints of altered sensorium since 3 days and fever, shortness of breath and a productive cough since 23 days
Timeline:
23 days ago:The patient was apparently asymptomatic 23 days ago when he went on a sudden alcohol binge for a couple of days following which he developed cough assosciated with sputum (scanty, non foul smelling, non sanguinous) and shortness of breath that could initially be classified under Class 2 NYHA(SOB with ordinary activity, slight limitation of physical activity) but gradually progressed to class 4(SOB at rest, severe limitation of physical activity). He also had burning sensation of the oral cavity that he recalls to have begun around the same time.
Following these complaints, the patient was taken to a nearby Government hospital, where he was trated symptomatically.
20 days ago: The patient was shifted to another local hospital where a chest X Ray was done and he was told he has viral pneumonia of the right lung.
3 days ago: The patient was brought to our hospital by his wife who said that she noticed a change in his responsiveness and slurring of speech that began 3 days ago. The patient presented to the casuality ward with some drowsiness, but he was arousable.
On examination of his oral cavity, multiple erythematous lesions are seen over his hard palate
PAST HISTORY
No similar complaints in the past.
No H/o DM ,HTN, TB, Asthma, epilepsy, CAD.
No known history of surgeries or blood transfusions.
FAMILY HISTORY
No history of similar illnesses among immediate family members.
The patient lost his first wife to an unknown illness 30 years ago. He has 2 daughters with his second wife.
No history of CKD, DM,HTN,CVA, TB, Asthma or CAD among his immediate family members.
PERSONAL HISTORY
The patient is married.
Diet: Mixed
Appetite: decreased recently
Sleep:Adequate
Bowel and bladder: Decreased urine output
No known drug allergies
He consumes 150ml of Alcohol every other day, his last intake was 23 days back.
GENERAL EXAMINATION
Patient is conscious, not coherant or cooperative, not oriented to time, place and person. He appears confused and irritated.
Moderately built and nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS:
Temperature: febrile on arrival
PR: 87 bpm
BP: 120/70 mmHg
RR: 24 cpm
SpO2: 98% with 4L of O2
GRBS: 229mg/dl
SYSTEMIC EXAMINATION:
CNS: E4V4M6
Sensory examination: Normal
Motor examination: Normal
Cranial nerve functions: intact
Speech: slurred
Kernig's sign: Positive
Brudzinski neck and leg signs: Negative
RS: B/L Crepts +, Dullness to percussion on right upper lobe, NVBS
CVS: S1, S2 heard, no murmurs
P/A: Soft, non tender
Erythematous lesions seen on the hard palate
Kernig's sign positive: Patient grimaced as the leg was being extended
Brudzinski sign: Negative
INVESTIGATIONS:
1) Hemogram (6/1/22)
2) Blood grouping and Rh type
07/01/22
08/01/22
4) Prothrombin time
07/01/22
08/01/22
5) ABG
6) HIV 1/2 Rapid test : Non reactive
7) HBsAg- Rapid
8) CUE
9) CBP
10) Blood fasting sugar (07/01/22)
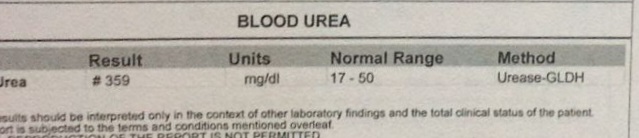
11) Blood Urea
12) Serum Creatinine
13) Serum Uric Acid
14) ECG
06/1/22, 7am
07/1/22, 11:12am and 11:16am
07/1/22, 7:50pm and 8:01pm
16) Covid RT-PCR: NEGATIVE (tested on arrival)
17) Sputum for AFB: NEGATIVE
18) Abdominal USG
PROVISIONAL DIAGNOSIS: Altered sensorium as a consequence of exacerbated uremic encephelopathy along with acute kidney injury secondary to sepsis, viral pneumonia of the right upper lobe in a 70 year old
TREATMENT:
1. MUCOPAIN Gel BD* 1 week
2. BETADINE mouth gargles TID* 1 week
3. Tab MVT OD* 15 days
4. Inj PIPTAZ 2.25gm TID
5. THIAMINE in 100ml normal saline TID
6. Tab AZITHROMYCIN 500mg*PO/OD
7. Inj LASIX 40mg IV BD
8. Tab Montek-LC
9. Tab ACEBROPHYLLINE
10. Tab Pulmoclear PO OD
11. Syp: Ambroxyl 15ml PO TID
12. Nebulizer with BUDECORT- 8th hourly
Duolin- 12th hourly
13. Inj HYDROCORTISONE 100mg IV stat
14. Inj VIT K 1 ampoule in 100ml NS for slow IV
Other measures: Head elevation
Vitals checked every 4hrs
O2 inhalation to maintain SpO2 greater than 94%
Monitor urinary output
GRBS every 6th hourly
Chest physiotherapy




















Comments
Post a Comment