Introduction: This is an online E-log Entry Blog to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs.
Note: The cases have been shared after taking consent from the patient/guardian. All names and other identifiers have been removed to secure and respect the privacy of the patient and the family.
Consent: An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
A 35-year-old male presented with the chief complaints of episodic dry cough and noisy breathing since 7 months.
History of Presenting Illness:
The patient was apparently asymptomatic 7 months ago when he first noticed a dry hacking cough and noisy breathing that was insidious in onset and gradually progressed to his current frequency.
He first went to a local physician who prescribed him a 1 week course of antibiotics. On noting no improvement, he went to a physician again who prescribed him a second week long course of antibiotics. This is his third visit for his ailment. The patient has had no previous imaging done.
The cough is aggravated by several factors:
- Cold weather/ AC rooms/ cold breeze hitting his face
- Exertion (when asked about the type of activity, he says riding his bike in the summer months or brisk walking to work makes it worse)
- Lying down/sleeping: he complains of severe cough and noisy breathing when he lies down to go to bed, to the extent where he cannot sleep and needs to sit upright or take a walk. He says taking a walk decreases his cough in such instances.
24/7/23: The patient couldn't sleep all night because of his cough.
Prolonged coughing leads to chest pain and shortness of breath in his case.
The patient complains of increased fatigue and weakness in the past 6-7 months. He says he has not had any weight changes as all his clothes fit him the same. He has had no changes in appetite.
History of past illness:
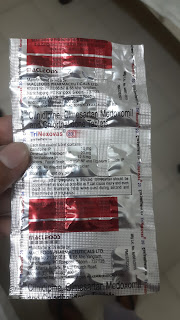
K/C/O Hypertension since 2 years.
Complains of occasional dry eyes at the end of the day.
Not a known case of DM, Asthma, TB, Epilepsy, CAD, CVD
Medication History:
He was prescribed this antihypertensive 2 years ago and has been taking it ever since.
The patient took 2 full courses of an unknown antibiotic 3 months ago.
Surgical history:
No surgical history
Personal history:
Normal appetite, mixed diet
Bowel movements: 1/day, normal in consistency.
Urine output: 2-3/day, no burning on micturition.
Occasional drinker, drinks 90ml of hard liquor once every 3-4 months.
Smokes 1-2 cigarettes/ month. He claims that his smoking has no effect on his cough and does not worsen it.
Has been chewing 1 packet of ghutka a day for the past 5 years.
Food and drug allergies: No known allergies.
Daily routine:
The patient lives with his wife, child, his mother and his two sisters. He is a software engineer and works close to home.
Patient's record: He wakes up at 7:50 and has a cup of tea before leaving to work at 9. He states that he has his first meal at 11am. He resumes work and takes his next break at 3pm, which is when he goes back home to take a shower. This is followed by his second meal at home. He goes back to work at around 5pm and stays there until 10pm. He has dinner between 11pm and 12am and goes to bed at 1am.
Wife and sister's account: He wakes up right before leaving to work, sometimes at 8. His daily schedule is very irregular, with his first meal being as late as 3pm sometimes. His sister claims that on some days he brushes his teeth at 11am and takes a bath at night. He has 2 meals on more days than he has 3.
On asking the patient to rate his level of day to day physical activity on a scale of 0-10, with 0 being no activity at all and 10 being athletic, the patient gave himself a 1.
Family History
No similar complaints in her family.
His father was diagnosed with tuberculosis 5 years ago for which he received treatment and was treatment success was confirmed that following year. His father passed away due to complications of covid infection in 2020. He was diabetic.
The patient's wife has had chest pain for the past 6 months and complains of increasing abdominal distension since her C- section in 2021. Her chest pain worsens at night.
General physical Exam:
On admission:
Vitals:
Afebrile (98.6)
BP: 110/70mmHg
HR: 80bpm
RR: 16cpm
SpO2: 98% on RA
GRBS: 107mg/dL
Patient is conscious, coherent and cooperative, well oriented to time, place and person.
No signs of pallor, cyanosis, icterus, lymphadenopathy, clubbing or pedal edema.
JVP normal
Systemic exam:
Cardiovascular System: S1, S2 heard, no murmurs.
Respiratory System: BAE+, VBS, stertor+ at the time of examination,
Per Abdomen: Soft and nontender, no organomegaly.
CNS: C/C/C, AOx3, no focal neurological defects, CN function intact.
Investigations: Patient has not consented to any investigations as of now.
Provisional diagnosis: Episodic paroxysmal cough in a known case of hypertension? Asthma?
Treatment:
TAB CETIRIZINE 10mg PO OD
TAB PANTOPRAZOLE 40mg PO OD before breakfast
TAB ULTRACET PO 1/2 QID




Comments
Post a Comment