This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 46 year old female who is a resident of Chintakunta and an agricultural labourer by occupation was brought to the casualty with chief complaints of sudden distension of abdomen and difficulty in breathing since 1 week.
History of presenting illness
2014: The patient started experiencing pain in both her knee joints along with restricted mobility. She says it was starting then that she couldn't sit from a standing position or stand from a sitting position with ease anymore.
2021: The patient was apparently asymptomatic 1 year back when she developed dyspepsia for which she was prescribed some PPIs which she started using on and off to treat her symptoms. The patient says she has developed an intolerance to spicy food this past year.
6th June,2022: i) The patient woke up in the morning and left to work as usual with no complaints, but at 6 in the evening, she started experiencing a sudden difficulty in breathing and had to sit down to recover. She said she felt like there was a huge weight on her chest that wasn't allowing her to breath in fully.
ii) She noted a distension in her epigastric and right hypochondriac region that was not present the day before. The swelling was not assosciated with pain.
iii) She also complained of severe bilateral knee pain that was apparently worsened during this period.
9th June.2022: She once again experienced a heart burn but this time it was not relieved by her regular medication.
10th June,2022: She was admitted to the hospital where she currently is.
12th June,2022: As of this day, the patient reports shortness of breath even at rest. Her knee pain is aggravated by walking and relieved by rest. Her abdominal swelling is assosciated with mild pain on the right side.
No history of cough, cold or fever
No H/o, loose stools , constipation, burning micturition
No chest pain, palpitations or PND .
No H/o headaches.
Past history:
- Patient has had bilateral knee pain and difficulty is standing up from sitting position since 5 years
- She is not a known case of Diabetes Mellitus,Hypertension, Asthma, CAD, hypothyroidism, TB, RA.
- No drug history.
- No history of other recent illnesses.
Surgical history:
The patient underwent a caeserian section during the birth of her second child and was tubectomized 16 years ago.
Daily routine:
The patient lives with her husband and son. She wakes up at 5 am everyday, cleans her house, prepares meals for her family and leaves to work at 9. She has lunch at 2pm. She returns home at 5pm and rests for half an hour before she starts with her household chores and preparation of dinner. She goes to bed at 10pm.
The patient spends many hours under direct sunlight and has handled chemicals and pesticides in the past without personal protective equipement. She wears slippers to work.
Personal History
Diet: Mixed
Appetite: Normal
Sleep: adequate
Bowel and Bladder movements: Regular
No known allergies
No known addictions, does not indulge in alcohol.
Menstrual history: Attained menopause last year (Has not had menstrual bleeding for 13 months)
Family History
No history of similar illnesses among immediate family members.
The patient is married and has one son and one daughter.
No history of DM,HTN,CVA, TB, Asthma or CAD among her immediate family members.
General examination
The patient is conscious, coherent, co-operative; well oriented to time, place and person.
Heavily built, well nourished.
No pallor, icterus,cyanosis, clubbing, lymphadenopathy, edema.
Bilateral non tender swelling around knee joints.

HR: 86 bpm
BP: 120/80 mmHg in both arms
RR: 20cpm
TEMP: 99°F
SpO2 at RA: 96%
Systemic Examination
RS: BAE+, NVBS
- The patient has grade 2 SOB (MMRC scale)
- Chest is symmetrical
- Trachea is central
- Chest expansion is symmetrical b/l
- Resonant on both sides
- No adventitious sounds heard
CVS: S1, S2 heard; no murmurs
P/A:
- Distended
- Palpable mass in the Epigastric region extending 5cm below the subcostal margin.
- No tenderness
- No fluid thrill or shifting dullness
- Normal Bowel sounds
- Liver is palpable.
Examination of the abdominal swelling:
- The swelling moves with respiration
- Cough impulse is positive
- There is no local rise of temperature
- Mild tenderness is present
CNS: Higher mental function : intact
Cranial nerve functions : normal and intact
Motor system:
•Muscle Bulk: Normal on inspection and palpation on all 4 limbs, uniform and symmetrical on right and left sides
Muscle tone: Normal in both upper and lower limbs on both the right and left sides
•Muscle power: Symmetrical on right and left sides, normal
upper limbs: 5/5
lower limbs: 5/5
•Reflexes: Both superficial and deep reflexes present and normal
No involuntary movements
Sensory system: Normal
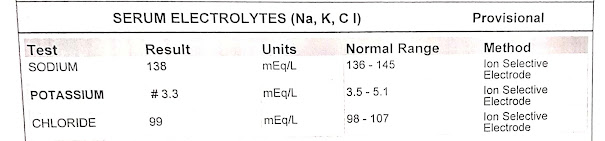
Investigations:
8PM: 282 mg/dl
6AM: 257 mg/dl


COLOUR DOPPLER 2D-ECHO
- Sclerotic Aortic Valve
- Good LV systolic function
ULTRASOUND REPORT
- 15mm defect noted in the Epigastrium with herniated contents( Omentum included)
- Grade 2 fatty liver
Provisional diagnosis: 46 year old female with abdominal distension, acid peptic disease and denovo type 2 Diabetes Mellitus currently undergoing conservative treatment.
Treatment:
INJ NPH: 4U AT 8AM AND 4U AND 8PM
INJ HAI: 6U AT 8AM, 6U AT 2PM, 6U AT 8PM
INJ PANTOPRAZOLE 40MG IV OD
TAB PARACETAMOL+TRAMADOL PO (1/2 TABLET) SOS
INJ OPTINEURON( B COMPLEX) IN 100ML NS IV OD





















Comments
Post a Comment