This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 30 year old female who is a resident of Nagarjunasagar and a homemaker was brought to the casualty with chief complaints of involuntary jerky movements in all 4 limbs.
History of presenting illness
17th March,2022: 12 days ago she developed fever which was insidious in onset, high in grade, gradually progressive and subsided on taking medication. It was accompanied with an occasional dry cough.
18th March,2022: She was taken to a local clinic the next day where the NS1 antigen test was ordered. The test was positive.
20th March,2022: Due to worsening of her joint pains and persistence of fever for the second day in a row she was admitted in the ICU of a local private hospital. There, a chest xray, cbp,lfts were ordered.
22nd March,2022: 1 unit of platelets were transfused due to a drop in her platelet count.
25th March,2022: She was discharged from the hospital and taken home
26th March,2022: The patient's mother noticed jerky involuntary movements in all 4 limbs of the patient early in the morning. There was associated drooling of saliva and the patient's eyes rolled upwards. No tongue biting.
This episode lasted for roughly 5 minutes and once it ended the patient did not seem to remember having the fit. There was no involuntary urination/defecation, vomiting after the episode.
She was taken to a different private hospital, where she is currently admitted.
28th March,2022: As of this day, the patient reports an improvement in her pain. She says that earlier her whole body hurt but now the pain is restricted to her calves only. She complains of a pain behind her sternum that increases on inspiration.
The patient also complains of some facial puffiness.
No history of Pain abdomen
No H/o, loose stools , giddiness, hematuria
No rash & bleeding manifestations .
No H/o retro orbital pain , joint pains
Past history:
- Patient had one episode of seizures 2 days after the delivery of her first child 5 years ago during which her consciousness was intact.
- She is not a known case of Diabetes, Hypertension, Asthma, CAD, hypothyroidism, TB, RA.
- No drug history.
- No history of other recent illnesses.
Daily routine:
The patient lives with her husband and 2 children. She wakes up at 6:30am everyday, gets her children ready for school while managing the chores. She has lunch at 1:30pm. She finishes the rest of her household work and has dinner at 8:30pm and goes to bed at 10pm everyday.
The patient notes that their neighborhood has a lot of mosquitoes around this time of the year.
Personal History
Diet: Mixed
Appetite: Normal
Sleep: adequate
Bowel and Bladder movements: Regular
No known allergies
No addictions
Menstrual history: She attained menarche at the age of 12. Her cycle has since been regular and lasts approximately 30 days. She bleeds for 4 days.
Menstruation that occurred after the onset of her current symptoms was accompanied by a slight increase in bleeding. No clots associated.
Family History
No history of similar illnesses among immediate family members.
The patient is married and has one son (5yo) and one daughter (3.5yo). Her husband and children did not test positive for the NS1 antigen.
No history of DM,HTN,CVA, TB, Asthma or CAD among her immediate family members.
General examination
The patient is conscious, coherent, co-operative; well oriented to time, place and person.
Moderately built, well nourished.
No pallor, icterus,cyanosis, clubbing, lymphadenopathy, edema.
Vitals
HR: 86 bpm
BP: 100/70 mmHg
RR: 20cpm
TEMP: Afebrile
SpO2 at RA: 98%
Fever chart of the patient
Systemic Examination
RS: BAE+, NVBS
- Chest is symmetrical
- Trachea is central
- Chest expansion is symmetrical b/l
- Dullness on percussion on the right side
- Decreased fremitus on the right
- Decreased breath sounds on the right
CVS: S1, S2 heard; no murmurs
P/A: soft, non tender, no organomegaly or ascites
CNS: Higher mental function : intact
Cranial nerve functions : normal and intact
Motor system:
•Muscle Bulk: Normal on inspection and palpation on all 4 limbs, uniform and symmetrical on right and left sides
•Measurements
upper limb 28.2 cms 28.2 cms
lower limb 30.7 cms 30.7cms
Muscle tone: Normal in both upper and lower limbs on both the right and left sides
•Muscle power: Symmetrical on right and left sides, normal
upper limbs: 5/5
lower limbs: 5/5
•Reflexes: Both superficial and deep reflexes present and normal
No involuntary movements
Sensory system: Normal
Kernigs sign: -ve
Brudzinski sign: -ve
Investigations:
COVID RTPCR NEGATIVE
NS1 Antigen test: Positive
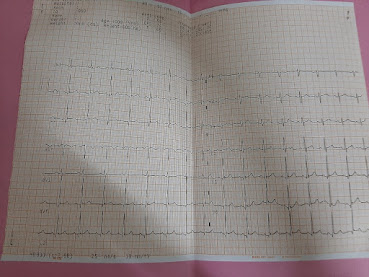
ECG:
MRI:
USG:
CXR:
Provisional diagnosis: 30 year old female with dengue fever, seizures and a right sided pleural effusion under observation.
Treatment:
INJ LEVETERACITAM 1gm in 100ml NS IV
INJ PANTOPRAZOLE 40 mg IV stat
IVF NORMAL SALINE, RINGER LACTATE 75 ml / hour with 1 amp of OPTINEURON
INJ PANTOPRAZOLE 40 mg IV per OD
INJ ONDANSETRON 4 mg /IV /sos
INJ NEOMOL Infusion 100ml (if temp> 101.1 ° F)
TAB PARACETAMOL 500 mg/PO/ TID
TAB LEVETERACITAM 500 mg PO/ BD
INJ LORAZEPAM 2cc/IV/SOS



























Comments
Post a Comment